It is an old aphorism: you cannot solve a problem at the level at which it was created.
There is also the more management-friendly version: every system is perfectly designed to produce the results it gets.
I still remember the feeling when the truth of this first landed for me.
Decades later, I see that this is only part of the truth.
These phrases tend to frame the problem as something actively produced: the problem is created by this; the system generates that result. And yes, that is often true.
Yet sometimes the deeper issue may be less the presence of something harmful, and more the absence of something essential.
Perhaps a little like malnutrition: the symptoms may not arise from what is present, but from what is missing.
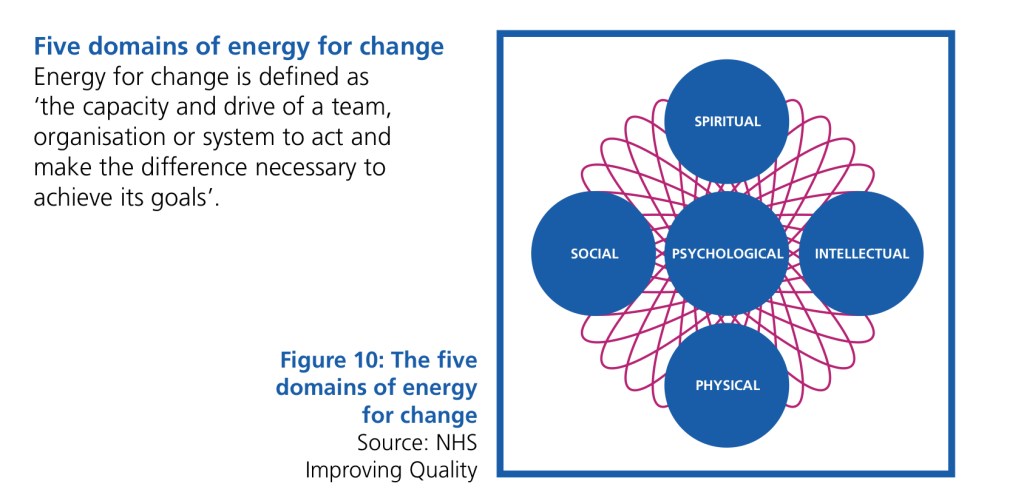
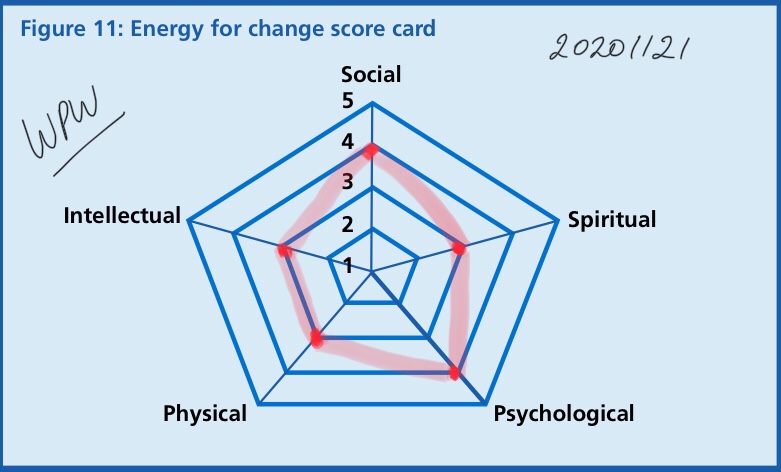
Over the years, I have found one image from Leading Large Scale Change to be foundational: the five domains of energy.
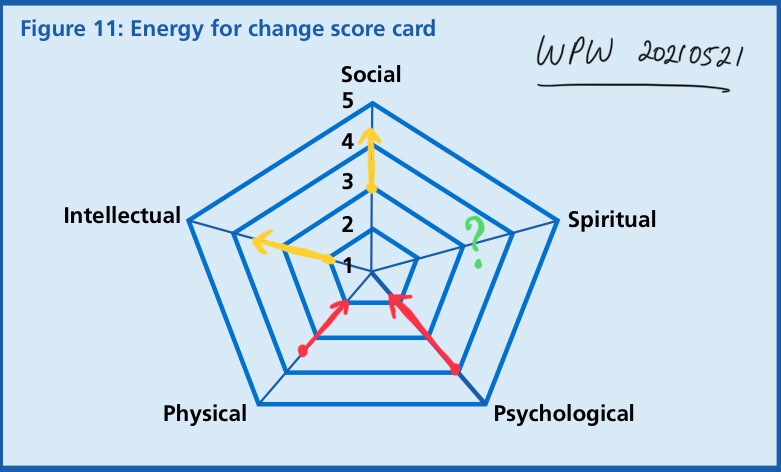
Across three decades, I have borne witness to the ever-increasing emphasis on physical, intellectual, social, and, more recently, psychological energies in efforts to improve health system outcomes.
And yet, it often seems that the more we do, the further we move from the outcomes we are trying to achieve.
Which leaves me wondering whether a deficit in spiritual energy is at the root of our limitations in health and social outcomes.
There are many reasons why spiritual energy has been de-recognised or de-emphasised in health and care. There is no blame in this. The reasons may be understandable in themselves.
Yet the outcomes in healthcare systems worldwide are clear, certainly in Emergency Medicine, the canary in the coal mine. The system cannot bear the growing strain and imbalance between capacity and patient demand.
I wonder – if a systemic problem arises from a lack of spiritual energy, can it really be improved by overcompensating with the other energies, or does that risk deepening the problem further ?
Over the coming weeks, I hope to share some reflections on what spiritual energy might be, and perhaps what it is not, in the context of healthcare.
Thank you for sharing this journey.